The Defense Innovation Unit is bringing together the
best of commercially available artificial intelligence technology and
the Defense Department's vast cache of archived medical data to teach
computers how to identify cancers and other medical irregularities.
The result will be new tools medical professionals can use to more
accurately and more quickly identify medical issues in patients.
The new DIU project, called "Predictive Health," also involves the
Defense Health Agency, three private-sector businesses and the Joint
Artificial Intelligence Center.
The new capability directly supports the development of the JAIC's
warfighter health initiative, which is working with the Defense Health
Agency and the military services to field AI solutions that are aimed at
transforming military health care. The JAIC is also providing the
funding and adding technical expertise for the broader initiative.
"The JAIC's contributions to this initiative have engendered the
strategic development of required infrastructure to enable AI-augmented
radiographic and pathologic diagnostic capabilities," said Navy Capt.
(Dr.) Hassan Tetteh, the JAIC's Warfighter Health Mission Initiative
chief. "Given the military's unique, diverse, and rich data, this
initiative has the potential to compliment other significant military
medical advancements to include antisepsis, blood transfusions, and
vaccines."
A big part of the Predictive Health project will involve training AI
to look at de-identified DOD medical imagery to teach it to identify
cancers. The AI can then be used with augmented reality microscopes to
help medical professionals better identify cancer cells.
Nathanael Higgins, the support contractor managing the program for DIU, explained what the project will mean for the department.
"From a big-picture perspective, this is about integrating AI into
the DOD health care system," Higgins said. "There are four critical
areas we think this technology can impact. The first one is, it's going
to help drive down cost."
The earlier medical practitioners can catch a disease, Higgins said,
the easier it will be to anticipate outcomes and to provide less
invasive treatments. That means lower cost to the health care system
overall, and to the patient, he added.
Another big issue for DOD is maximizing personnel readiness, Higgins said.
"If you can cut down on the number of acute issues that come up that
prevent people from doing their job, you essentially help our
warfighting force," he explained.
Helping medical professionals do their jobs better is also a big part of the Predictive Health project, Higgins said.
"Medical professionals are already overworked," he said. "We're
essentially giving them an additional tool that will help them make
confident decisions — and know that they made the right decision — so
that we're not facing as many false negatives or false positives. And
ultimately we're able to identify these types of disease states earlier,
and that'll help the long-term prognosis."
In line with the department adding an additional line of effort
focused on taking care of people to the National Defense Strategy,
Higgins said using AI to identify medical conditions early will help to
optimize warfighter performance as well.
"Early diagnosis equals less acute injuries, which means less
invasive procedures, which means we have more guys and gals in our
frontline forces and less cost on the military health care system," he
said. "The ultimate value here is really saving lives as people are our
most valuable resource."
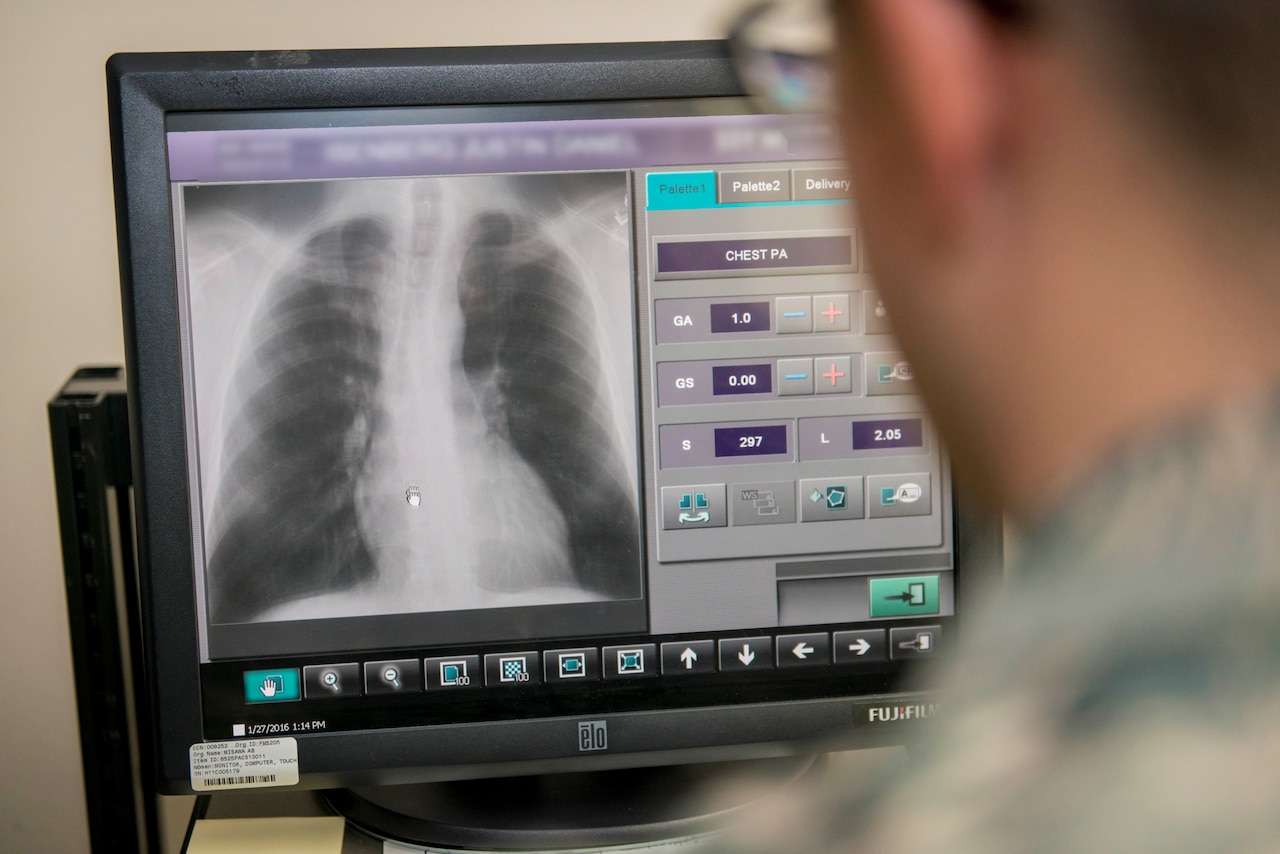
Using AI to look for cancer first requires researchers to teach AI
what cancer looks like. This requires having access to a large set of
training data. For the Predictive Health project, this will mean a lot
of medical imagery of the kind produced by CT scans, MRIs, X-rays and
slide imagery made from biopsies, and knowing ahead of time that the
imagery depicts the kind of illnesses, such as cancer, that researchers
hope to train the AI to identify.
DOD has access to a large set of this kind of data. Dr. Niels Olson,
the DIU chief medical officer and originator of the Predictive Health
project, said DOD also has a very diverse set of data, given its size
and the array of people for which the department's health care system is
responsible.
"If you think about it, the DOD, through retired and active duty
service, is probably one of the largest health care systems in the
world, at about 9 million people," Olson said. "The more data a tool has
available to it, the more effective it is. That's kind of what makes
DOD unique. We have a larger pool of information to draw from, so that
you can select more diverse cases."
"Unlike some of the other large systems, we have a pretty good
representation of the U.S. population," he said. "The military actually
has a nice smooth distribution of population in a lot of ways that other
regional systems don't have. And we have it at scale."
While DOD does have access to a large set of diverse medical imaging
data that can be used to train an AI, Olson said privacy will not be an
issue.
"We'll use de-identified information, imaging, from clinical
specimens," Olson said. "So this means actual CT images and actual MRI
images of people who have a disease, where you remove all of the
identifiers and then just use the diagnostic imaging and the actual
diagnosis that the pathologist or radiologist wrote down."
AI doesn't need to know who the medical imaging has come from — it
just needs to see a picture of cancer to learn what cancer is.
"All the computer sees is an image that is associated with some kind
of disease, condition or cancer," Olson said. "We are ensuring that we
mitigate all risk associated with [the Health Insurance Portability and
Accountability Act of 1996], personally identifiable information and
personal health information."
Using the DOD's access to training data and commercially available AI
technology, the DIU's Predictive Health project will need to train the
AI to identify cancers. Olson explained that teaching an AI to look at a
medical image and identify what is cancer is a process similar to that
of a parent teaching a child to correctly identify things they might see
during a walk through the neighborhood.
"The kid asks 'Mom, is that a tree?' And Mom says, 'No, that's a
dog,'" Olson explained. "The kids learn by getting it wrong. You make a
guess. We formally call that an inference, a guess is an inference. And
if the machine gets it wrong, we tell it that it got it wrong."
The AI can guess over and over again, learning each time about how it
got the answer wrong and why, until it eventually learns how to
correctly identify a cancer within the training set of data, Olson said,
though he said he doesn't want it to get too good.
Overtraining, Olson said, means the AI has essentially memorized the
training set of data and can get a perfect score on a test using that
data. An overtrained system is unprepared, however, to look at new
information, such as new medical images from actual patients, and find
what it's supposed to find.
"If I memorize it, then my test performance will be perfect, but when
I take it out in the real world, it would be very brittle," Olson said.
Once well trained, the AI can be used with an "augmented reality
microscope," or ARM, so pathologists can more quickly and accurately
identify diseases in medical imagery, Olson said.
"An augmented reality microscope has a little camera and a tiny
little projector, and the little camera sends information to a computer
and the computer sends different information back to the projector,"
Olson said. "The projector pushes information into something like a
heads-up display for a pilot, where information is projected in front of
the eyes."
With an ARM, medical professionals view tissue samples with
information provided by an AI overlaid over the top — information that
helps them more accurately identify cells that might be cancerous, for
instance.
While the AI that DIU hopes to train will eventually help medical
professionals do a better job of identifying cancers, it won't replace
their expertise. There must always be a medical professional making the
final call when it comes to treatment for patients, Higgins said.
"The prototype of this technology that we're adopting will not
replace the practitioner," he said. "It is an enabler — it is not a
cure-all. It is designed to enhance our people and their decision
making. If there's one thing that's true about DOD, it's that people are
our most important resource. We want to give them the best tools to
succeed at their job.
"AI is obviously the pinnacle of that type of tool in terms of what
it can do and how it can help people make decisions," he continued. "The
intent here is to arm them with an additional tool so that they make
confident decisions 100% of the time."
The Predictive Health project is expected to end within 24 months,
and the project might then make its way out to practitioners for further
testing.
The role of DIU is taking commercial technology, prototyping it
beyond a proof of concept, and building it into a scalable solution for
DOD.