A vial of Moderna COVID-19 vaccine is seen at Royal Air Force Lakenheath, England, Dec. 29, 2020, when the 48th Medical Group conducted its first inoculations of health care workers with the vaccine.
“It has become appallingly obvious that our technology has exceeded our humanity.” Albert Einstein
A vial of Moderna COVID-19 vaccine is seen at Royal Air Force Lakenheath, England, Dec. 29, 2020, when the 48th Medical Group conducted its first inoculations of health care workers with the vaccine.
Below is a compilation of initiatives, actions and accomplishments across Operation Warp Speed (OWS)’s primary efforts in the past week. To learn more about OWS, visit the Department of Health and Human Services (HHS) website and Department of Defense (DOD) website.
2020 RECAP
Here is a look back at the accomplishments of Operation Warp Speed since its inception in May. As the year closed out, more than 20 million doses of vaccines were allocated to jurisdictions and more than 14 million were delivered across states, territories and to five federal entities.
VACCINE DEVELOPMENT:
Novavax announced the start of its Phase 3 study in the U.S. and Mexico to evaluate the efficacy and safety of its COVID-19 vaccine. The trial builds on research from Phase 1 and 2 studies demonstrating that the vaccine provoked a robust immune response, generated highly neutralizing antibodies against the virus and was generally well-tolerated.
THERAPEUTICS DEVELOPMENT:
As of Wednesday, the U.S. government has allocated over 530,000 monoclonal antibodies to the U.S. healthcare system. States and territories can allocate these drugs to a variety of settings: hospitals, alternate care facilities, infusion centers, long-term care facilities, and other outpatient facilities. About 80% of these treatment courses remain available to help decrease the need for our most vulnerable patients from being hospitalized for COVID-19.
MANUFACTURING, DISTRIBUTION AND ADMINISTRATION:
Operation Warp Speed accelerated vaccine manufacturing by selectively applying the authorities in the Defense Production Act. Priority ratings using the Defense Priorities and Allocations System and Health Resources Priorities and Allocations System were used 18 times to help manufacturers secure the raw material and components necessary to produce COVID-19 vaccines and therapeutics.
KEY ENGAGEMENTS/OUTREACH:
Operation Warp Speed leaders made several visits to administration sites including Holy Cross Hospital in Maryland and Walter Reed, to observe the vaccine ordering and administration process in various settings.
Operation Warp Speed leaders provided updates and addressed vaccine distributions in a regular weekly press briefing. The next briefing is set for Jan. 6. Sign up for email updates.
SENIOR LEADER QUOTES:
“Operation Warp Speed delivered by the end of 2020 two FDA-authorized antibody treatments, two FDA-authorized vaccines, five vaccine candidates in Phase 3 clinical trials, and 20 million first doses of vaccine allocated, with the second doses on hand ready to be shipped a few weeks later. This is unprecedented and historic. I am grateful to everyone who has worked tirelessly on this effort this year to save lives.”—Health and Human Services Secretary Alex Azar
“Reflecting on the past seven months, I am so grateful for the men and women who are supporting this effort across the country - from the front lines to the manufacturing facilities. Our country has never done this before, and the dedication at all levels is powerful.” ~ Operation Warp Speed Chief Operation Officer Army Gen. Gus Perna
“I want to join General Perna in thanking and acknowledging the work of tens of thousands of people in the development, manufacture and supply vaccine and administration of the vaccine,” ~ Operation Warp Speed Chief Science Advisor Dr. Moncef Slaoui
Operation Warp Speed is a partnership among components of the Department of Health and Human Services and the Department of Defense, engaging with private firms and other federal agencies, and coordinating among existing HHS-wide efforts to accelerate the development, manufacturing and distribution of COVID-19 vaccines, therapeutics and diagnostics.Dec. 31, 2020 | BY Sarah Marshall, Uniformed Services University
Researchers at the Uniformed Services University of the Health Sciences recently identified pint-sized antibodies, or "nanobodies," that could protect against COVID-19. At least one of these nanobodies — produced by a llama named Cormac — also appears to work well in either liquid or aerosol form, suggesting it could also help protect a person's lungs from infections.

The study was led by Dr. David Brody, director of USU's Center for Neuroscience and Regenerative Medicine, along with Thomas J. "T.J." Esparza, a Henry M. Jackson Foundation for the Advancement of Military Medicine employee working in support of CNRM. Both Esparza and Brody also work in the National Institutes of Health's National Institute of Neurological Disorders and Stroke .
Nanobodies are a type of antibody naturally produced by the immune systems of camelids, such as camels, alpacas and llamas. These proteins are about a tenth of the weight of most human antibodies on average. They can be isolated in the lab and essentially free-floating versions of the tips of the arms of heavy chain proteins, which form the backbone of a typical Y-shaped human immunoglobulin antibody found in the blood. These tips recognize proteins on viruses, bacteria and other invaders, also known as antigens. Therefore, they play a vital role in the immune system's defenses.
Nanobodies are also more stable, less expensive to produce and easier to engineer than typical antibodies. Therefore, they have been increasingly used for medical research. A few years ago, for example, scientists showed humanized nanobodies may be more effective at treating an autoimmune form of thrombotic thrombocytopenic purpura, a rare blood disorder, than current treatments.
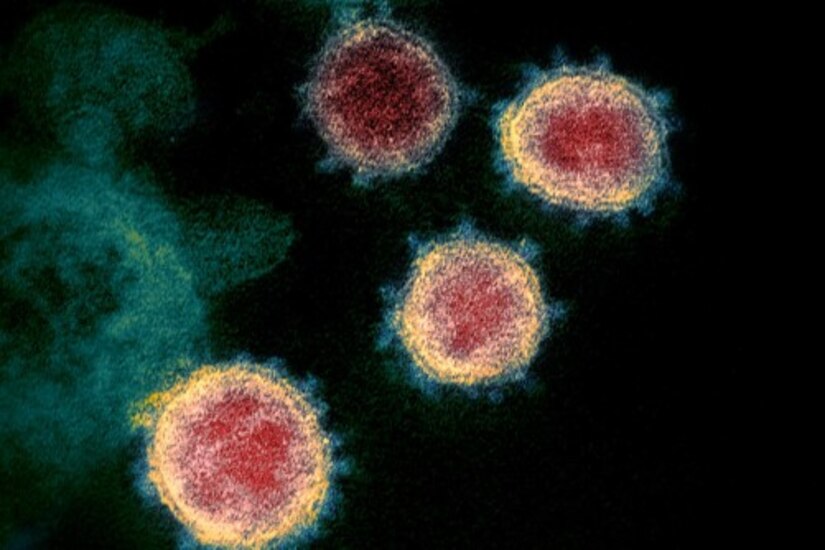
Since the pandemic broke, several researchers have produced llama nanobodies against the SARS-CoV-2 spike protein, which is believed to be effective at preventing infections. In this study, published in Scientific Reports, the researchers used a slightly different strategy to find nanobodies that may work especially well.
"For years, TJ and I had been testing out how to use nanobodies to improve brain imaging. When the pandemic broke, we thought this was a once in a lifetime, all-hands-on-deck situation and joined the fight," Brody, the senior author of the study, said. "We hope that these anti-COVID-19 nanobodies may be highly effective and versatile in combating the coronavirus pandemic."
The researchers found that at least one of these nanobodies, called NIH-CoVnb-112, may be highly effective at preventing infections or detecting virus particles by grabbing hold of SARS-CoV-2 spike proteins. These "spike proteins" act like a key by "opening the door to infections" when they bind to a protein found on the surface of certain cells, called the angiotensin converting enzyme 2 receptor, the researchers explained. They then found a way to isolate these nanobodies that block infections by covering the "teeth" of the spike protein, which bind to and unlock the ACE2 receptor. This was done by immunizing the llama, Cormac, five times over the course of 28 days with a purified version of the SARS-CoV-2 spike protein.
After testing hundreds of nanobodies, they found Cormac produced 13 nanobodies that could potentially be strong candidates, including one they refer to as NIH-CoVnB-112. The researchers then showed that the NIH-COVnB-112 nanobody could be effective at preventing infections.
To mimic the COVID-19 virus, the researchers genetically mutated a harmless 'pseudovirus' so that it could use the SARS-CoV-2 spike protein to infect cells that produce human ACE2 receptors. The researchers saw that relatively low levels of the NIH-CoVnb-112 nanobodies prevented the pseudovirus from infecting these cells in petri dishes.
Additionally, the researchers showed that the nanobody was just as effective in preventing the infections in petri dishes when it was sprayed through a nebulizer, or inhaler, often used to help treat patients with asthma.
"One of the exciting things about nanobodies is that, unlike most regular antibodies, they can be aerosolized and inhaled to coat the lungs and airways," Brody said. "This is promising in that it could potentially be used to protect the lungs from infections."
This study was supported by NIH Intramural Research Programs at the National Institute of Neurological Disorders and Stroke and National Institute of Environmental Health Sciences.
Dec. 29, 2020
Operation Warp Speed (OWS) continues to accelerate development of safe and effective vaccines by supporting multiple candidates. In line with this unprecedented effort, Womack Army Medical Center, is the latest Department of Defense (DOD) location to join Phase 3 SARS-CoV-2 vaccine trials. This location has been identified to participate in the Phase 3 clinical trial evaluating the safety and efficacy of the Novavax vaccine candidate NVX-CoV2373.
The Phase 3 clinical trial design is harmonized with those of other leading companies and calls for the enrollment of up to 30,000 participants in the U.S. and Mexico. This clinical trial expects to include proportional representation among diverse populations most vulnerable to COVID-19 distributed across race/ethnicity, age and those living with co-morbidities. Participants will randomly receive either the investigational vaccine or placebo in two doses, 21 days apart. Two-thirds of volunteers will receive the investigational vaccine and one-third will receive the placebo.
“‘We are extraordinarily appreciative of volunteers who are willing to roll up their sleeves and help fight this pandemic,” said Dr. Matt Hepburn, the vaccine development lead for Operation Warp Speed. “That same spirit of volunteerism is the foundation of military service.”
Anyone wishing to volunteer to participate in any OWS Phase 3 vaccine or monoclonal antibody prevention trial should visit www.CoronavirusPreventionNetwork.org, click on “Volunteer Now” and complete the survey. Once the survey is completed, local study site coordinators will contact Military Health System beneficiary volunteers in their area who are a good match for participation in the study.
To assist in the screening process for the DOD locations, each site is assigned a site code that should be entered during the process. Military Health System beneficiaries can also contact the site team directly. For the Novavax clinical trial location the Coronavirus Prevention Network (CoVPN) site code for Womack Army Medical Center is WAMC. Military Health System beneficiaries interested in participating can also contact the site team directly at covidwamc@genevausa.org or 253-316-3436.
“We greatly appreciate the effort and expertise of the DOD clinical teams in implementing the clinical research at the highest ethical and quality standards”, added Hepburn. “These clinical trials are essential in assessing these vaccines which are our best hope to end this pandemic.”
Womack (located on Fort Bragg, North Carolina) joins the five DOD facilities supporting the AstraZeneca Phase 3 trial, which is currently enrolling study participants in the United States. The codes and contact information for those locations are:
To ensure that the vaccines work to protect those at greatest risk, participation by people from communities that are hardest hit is critical. The studies are seeking participants who are at an increased risk of SARS-CoV-2 infection, which may include:
OWS is an U.S. government, interagency endeavor that is focused on delivering 300 million doses of a safe, effective vaccine for COVID-19 and is part of a broader strategy to accelerate the development, manufacturing, and distribution of vaccines, therapeutics, and diagnostics (countermeasures) for the virus.
Direct support for this effort is provided by the U.S. Department of Defense's (DOD) Joint Program Executive Office for Chemical, Biological, Radiological and Nuclear Defense (JPEO-CBRND) in coordination with the Office of the Assistant Secretary of Defense for Health Affairs (OASD(HA))and the Defense Health Agency (DHA).
Dec. 28, 2020 | BY Elaine Sanchez , Brooke Army Medical Center
Kathlyn Chassey was shocked when she was diagnosed with COVID-19 after experiencing a low-grade fever and a bad headache, Joint Base San Antonio-Fort Sam Houston, Texas, Dec. 21, 2020.

A former lung transplant recipient, Chassey had been staying close to home for months to avoid the respiratory risks associated with the virus. She figured she had an infection or the flu when she arrived at Brooke Army Medical Center's emergency department.
"When the doctor told me I had COVID-19, I had a panic attack because I'm extremely high risk, and I know what COVID-19 can do," Chassey, who had undergone a lung transplant in December 2016, said.
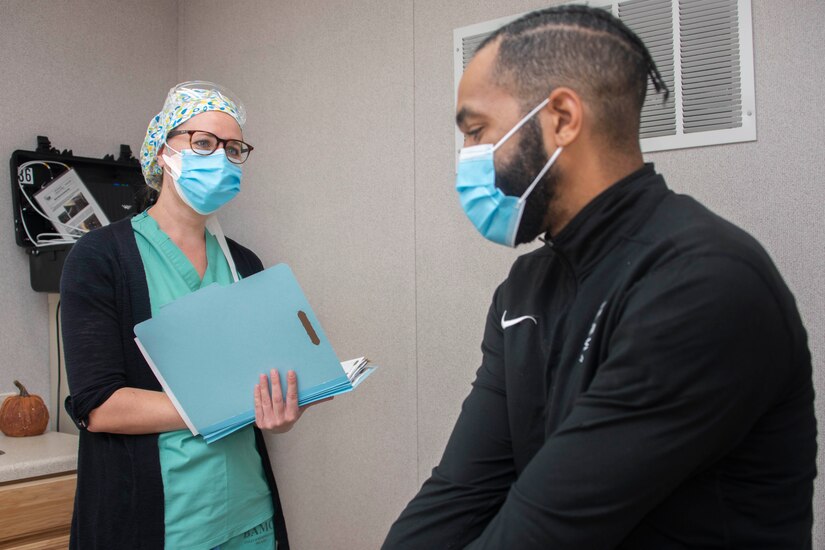
Fortunately, the 28-year-old had a mild case of COVID-19 and was ready to be discharged after a day in the hospital. However, due to her medical history, her medical team didn't want to send her home empty-handed.
Chassey became one of the first BAMC patients to be enrolled in the new COVID-19 Remote Monitoring Program, a joint effort of the Virtual Medical Center and BAMC. The program equips COVID-19 patients needing additional monitoring with a home health care kit and 24/7 oversight from registered nurses to ensure a higher level of post-hospital care.
"This is an exciting and unique new capability," Army Maj. Daniel Yourk, deputy director for operations, Virtual Medical Center, said. "We are able to move our patients from an inpatient to a home setting with round-the-clock monitoring and reach-back care."
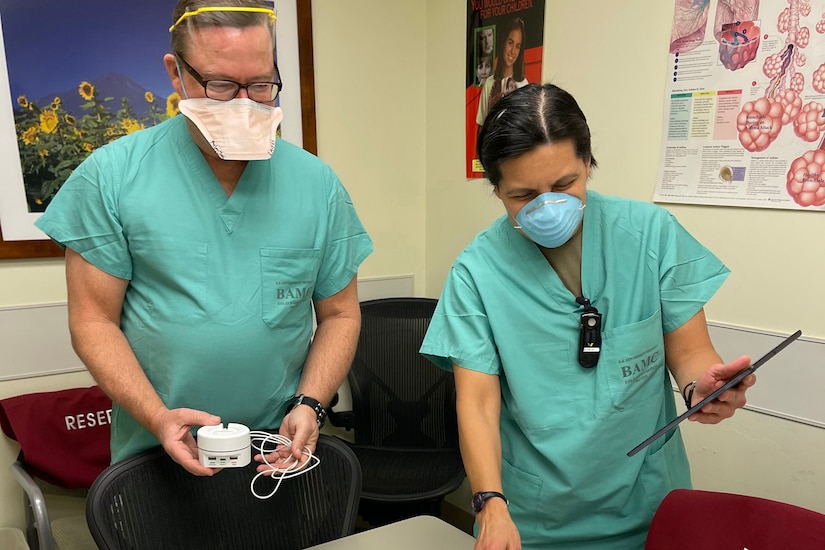
Through the use of the home kit and self-assessments, health care professionals are able to provide continuous monitoring of a patient's temperature, respiratory rate, heart rate and oxygen saturation with intermittent monitoring of blood pressure and spirometry, which measures the movement of air in and out of the lungs. The system also enables secure video consultations.
In effect, the program "bridges the continuum of care" from inpatient to outpatient, Army Lt. Col. Robert Walter, the program's clinical lead and BAMC's chief of pulmonary and critical care medicine, said. "We are offering an additional level of safety, support and monitoring."
The pilot concept, first developed by the Virtual Medical Center and BAMC, now spans the services and the nation. Participating military treatment facilities include Naval Medical Center San Diego, California; Madigan Army Medical Center, Joint Base Lewis McChord, Washington; Walter Reed National Military Medical Center, Bethesda, Maryland; Mike O' Callaghan MMC, Nellis Air Force Base, Nevada; David Grant U.S. Air Force Medical Center, Travis Air Force Base, California; Carl R. Darnall AMC, Fort Hood, Texas; and Fort Belvoir Community Hospital, Virginia.
The process starts in the hospital inpatient unit or emergency department prior to discharge and in consultation with designated providers at each MTF. If the patient qualifies for enrollment, they are equipped with the FDA-approved home monitoring kit and detailed verbal and printed instructions. The kit contains a tablet, a network hub that operates independently of Wi-Fi and an arm band containing a coin-sized monitor. The system also pairs with a blood pressure cuff, a temperature patch and a spirometer. Patients fill out customized questionnaires daily to report how they are feeling. Together, the system enables continuous bio-physiologic and symptom-based monitoring.
"Real-time data is compiled into a single dashboard where we can review all patients, grouped by risk," Walter explained.
A team of teleworking nurses, located in the San Antonio area, monitor patients across the eight participating MTFs. Additionally, each site has on-call medical staff in case of an alert or patient concern. Each tablet has a button for assistance that initiates nurse engagement and, if needed, a Health Insurance Portability and Accountability-compliant connection for face-to-face video evaluation with a nurse or on-call physician.
"I felt secure knowing the nurses were keeping an eye on me," Chassey said. "One night I was having a nightmare. They texted me because my heartrate had increased and wanted to know if I was ok. It's like being in the hospital, but in the comfort of your own home."
After a patient no longer needs monitoring or requires a higher level of inpatient care, the patient receives prepaid shipping boxes to pack up the equipment and calls a courier for a contactless pickup. The company then sanitizes, services and repackages the kit for mailing back to the MTF.
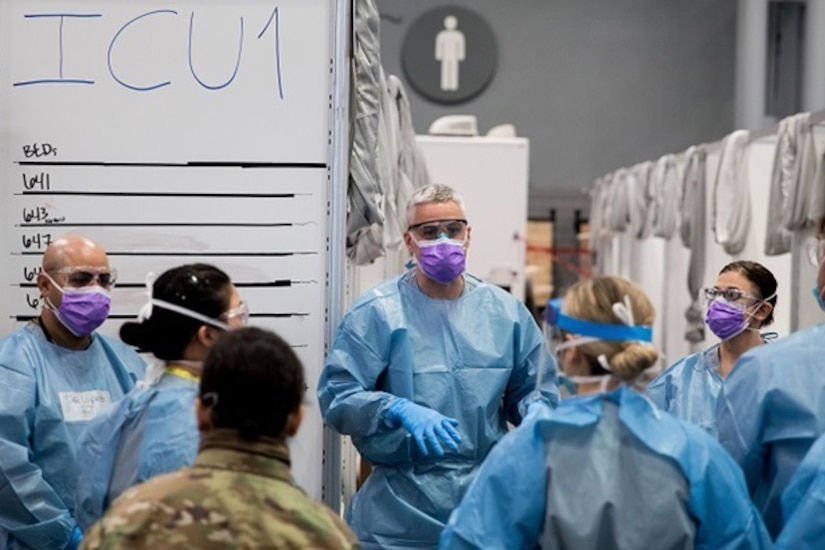
The idea for the program was spurred by lessons learned in New York last spring during the initial COVID-19 wave, Walter explained. "The hospitals were so busy; they were having to move patients through the continuum of care, from inpatient to outpatient, at a more rapid pace to accommodate incoming COVID-19 patients."
Some of these patients were still symptomatic or had higher oxygen requirements, he said, but with new patients flowing in, the care teams were faced with tough decisions. To mitigate risk, some hospital systems established a program in which paramedics would check on patients in their home to ensure they weren't declining or needing readmission.
"Reflecting on these experiences, we began to explore the idea of leveraging virtual health in the event we are faced with a COVID-19 surge in the hospital and need to move patients more quickly through the facility," Walter said. "If that happens, it becomes vital to retain capacity without compromising the safety or quality of care for our patients."
With a global vs. local program in mind, Walter and Yourk approached the Defense Health Agency, which assisted in obtaining and funding 200 home kits that could satisfy the requirement of a "high fidelity of monitoring in an outpatient environment," Walter said.
"It is truly incredible how the clinical leads from each military treatment facility and the Virtual Medical Center came together to take this pilot from a concept to reality in under six months to support beneficiaries from the East to West coast," Yourk added.
With the ongoing threat of the pandemic and to preserve bed capacity, the program is mainly intended for COVID-19 patients at this time, but there is a much broader application potential, Walter noted.
"We are exploring the long-term benefit for a number of conditions that often require frequent admissions, such as congestive heart failure, chronic obstructive pulmonary disease, cystic fibrosis and asthma," he said. "As with COVID-19 patients, the system can alert us to issues, enabling us the ability to adjust a care plan or facilitate a more rapid assessment if someone's condition worsens."
An additional population is patients who come to the emergency department who may not meet admission criteria, but could still benefit from elevated care, he added. Further down the line, Yourk hopes the program can be expanded to deployed service members and pediatric patients.
In the meantime, Walter and Yourk are focused on ensuring each MTF has the tools and support needed to successfully carry out this program, particularly as COVID-19 rates increase across the nation. The program will roll out in a phased approach to gauge the efficacy of the system, Walter said, before expanding to additional MTFs.
"We are truly at the leading edge," he noted. "There are well-validated use cases for single-data monitoring platforms, such as for patients with specific medical conditions such as heart arrhythmia, but we're helping break ground on a system that can monitor a number of different data points simultaneously for patients with varying diagnoses in the comfort of their home."
The kits have been disbursed to participating hospitals and 13 patients were enrolled in the first week, saving approximately 15 bed-days and improving the care delivered to patients, Yourk said.
Chassey said she's now on the road to recovery and is thankful for the safety net the remote patient monitoring pilot offered.
"I felt safer going home knowing that I had assistance standing by. I know from experience how quickly things can take a bad turn," she said.
"I wish I had something like this before my transplant," she added. "I spent so much time in the hospital over the years, and this type of technology would have given me more time at home."
Walter said the program is mutually beneficial. "This program enables patients to return home sooner, be with family, while mitigating COVID-19 risks to patients and staff," he said. "It's a game-changer for us as we continue to battle this pandemic."
Dec. 23, 2020
On December 23, 2020, the Department of Defense (DOD), in coordination with Department of Health and Human Services (HHS), awarded a $15 million Firm Fixed Price contract to Corning Incorporated to expand domestic production of pipette tips for robotic liquid handling instruments.
This industrial base expansion effort will allow Corning Life Sciences to increase production capacity of pipette tips for robotic liquid handling instruments at their Durham, North Carolina, facility by an additional 684 million pipette tips per year by October 2021. These tips can be used in a number of research and diagnostic applications, most notably in support of domestic COVID-19 testing.
The DOD’s Defense Assisted Acquisition (DA2) Cell led this effort in coordination with the Department of the Air Force’s Acquisition COVID-19 Task Force (DAF ACT). This effort was funded through Health Care Enhancement Act (HCEA) to enable and support domestic industrial base expansion for critical medical resources.
More information on today’s contracts can be found here.
Dec. 23, 2020
The Trump Administration, through the U.S. Department of Health and Human Services (HHS) and Department of Defense (DOD), will purchase an additional 100 million doses of COVID-19 vaccine from Pfizer.
On Dec. 11, the U.S. Food and Drug Administration (FDA) authorized the vaccine for emergency use and doses began shipping immediately. The vaccine is being provided at no cost to Americans. Vaccine administration costs for private-sector administration partners are covered by healthcare payers: private insurance, Medicare or Medicaid, and HHS’s program to cover COVID-19 costs for the uninsured which is reimbursing the provider at Medicare rates from the provider relief fund.
Under the agreement, Pfizer will manufacture and deliver up to 100 million doses of its SARS-CoV-2 vaccine, BNT162b2, to Government designated locations. Under the terms of the agreement, Pfizer will deliver at least 70 million doses by June 30, 2021, with the balance of the 100 million doses to be delivered no later than July 31, 2021.
The additional doses ordered today provide for a seamless transition from the first 100 million doses contracted earlier this year. This represents successful implementation of the U.S. government’s overall strategy to ensure continued availability of safe and effective SARS-CoV-2 vaccines to Americans. This strategy began in spring 2020 with Operation Warp Speed (OWS) planning and has been consistent in all initial OWS contracts and agreements with industry partners supporting large scale manufacturing of SARS-CoV-2 vaccines.
Today’s agreement also includes options for an additional 400 Million doses of the Pfizer vaccine. As part of ongoing coordination, the government and Pfizer are also continuing to discuss potential approaches to further strengthen our partnership and safely expand output and accelerate production.
“Securing more doses from Pfizer and BioNTech for delivery in the second quarter of 2021 further expands our supply of doses across the Operation Warp Speed portfolio,” said HHS Secretary Alex Azar. “This new federal purchase can give Americans even more confidence that we will have enough supply to vaccinate every American who wants it by June 2021.”
The agreement announced today brings the total doses of Pfizer’s vaccine purchased by the federal government to 200 million. Pfizer began manufacturing the first 100 million doses while clinical trials were underway. Manufacturing in parallel with clinical trials expedited the traditional vaccine development timeline and built toward the U.S. government’s Operation Warp Speed goal to begin delivering safe and effective vaccines to the American people by the end of the year. This goal has been achieved with the initial distribution of the Pfizer vaccine beginning immediately after the Food and Drug Administration granted Emergency Use Authorization (EUA).
The Biomedical Advanced Research and Development Authority (BARDA), part of the HHS Office of the Assistant Secretary for Preparedness and Response, has now collaborated with the DOD Joint Program Executive Office for Chemical, Biological, Radiological and Nuclear Defense (JPEO-CBRND) and Army Contracting Command - New Jersey to provide Pfizer approximately $4B total for the delivery of 200 million doses of the vaccine to Government-designated locations across the country.
The Pfizer vaccine was developed using messenger RNA, also called mRNA; mRNA vaccines take advantage of the process that cells use to make proteins in order to trigger an immune response and build immunity to a virus. In contrast, most vaccines use weakened or inactivated versions or components of a disease-causing virus to stimulate the body’s immune response to create antibodies.
About Operation Warp Speed
OWS is a partnership among components of the Department of Health and Human Services and the Department of Defense, engaging with private firms and other federal agencies, and coordinating among existing HHS-wide efforts to accelerate the development, manufacturing, and distribution of COVID-19 vaccines, therapeutics, and diagnostics.
Dec. 23, 2020
The U.S. Department of the Health and Human Services (HHS) and the Department of Defense (DOD) jointly announced an agreement with Merck to support advanced development and large-scale manufacturing of the their investigational therapeutic MK-7110 to treat hospitalized patients with severe or critical COVID-19.
The investigational therapeutic is a promising first-in-class fusion protein and immune modulator. Immune modulators have the potential to minimize the damaging effects of an overactive immune response to COVID-19. This overactive response can contribute to the severity of the illness.
“Our agreement with Merck is the latest example of how industry and government are coming together under Operation Warp Speed to move potential therapeutics all the way from development through to manufacturing, enabling faster distribution,” said HHS Secretary Alex Azar. “More good news about COVID-19 therapeutics is constantly emerging, and President Trump’s commitment to supporting lifesaving therapeutics has already helped deliver hundreds of thousands of Operation Warp Speed-supported therapeutics to the frontlines.”
The Biomedical Advanced Research and Development Authority (BARDA), part of the HHS Office of the Assistant Secretary for Preparedness and Response, collaborated with the DOD Joint Program Executive Office for Chemical, Biological, Radiological and Nuclear Defense (JPEO-CBRND) and Army Contracting Command (ACC-APG), to provide approximately $356 million to Merck. This funding allows for development of MK-7110, including completing activities required to request Emergency Use Authorization (EUA) from the U.S. Food and Drug Administration (FDA), and for delivery of up to 100,000 doses of MK-7110 by June 30, 2021.
With this approach, doses will be packaged and ready to ship in the first half of 2021, in the event FDA determines MK-7110 meets the statutory criteria for issuance of an EUA. The federal government would allocate these doses to treat severe and critical COVID-19 patients using the same approach that has been used successfully to allocate supplies of other COVID-19 therapeutic treatments. The doses will be made available to the American public at no cost. However, there may be costs associated with hospitalization.
Interim analysis of a Phase 3 clinical trial in September 2020 indicated that patients who received a single dose of the therapeutic had a 60 percent greater chance of clinical recovery than those who received a placebo. Preliminary analysis also showed that the treatment potentially reduces the risk of respiratory failure or death by 50 percent compared to the standard of care. The study is still ongoing.
About Operation Warp Speed (OWS):
OWS is a partnership among components of the Department of Health and Human Services and the Department of Defense, engaging with private firms and other federal agencies, and coordinating among existing HHS-wide efforts to accelerate the development, manufacturing, and distribution of COVID-19 vaccines, therapeutics, and diagnostics.
Army Spc. Ying Chen, a New York National Guardsman, prepares a dosage of the Pfizer-BioNTech COVID-19 vaccine at the Camp Smith Training Site Medical Readiness Clinic, N.Y., Dec. 18, 2020. The New York National Guard is administering 44,000 doses of the Pfizer vaccine to front line medical personnel at 16 locations around the world as part of a pilot program.
An Oregon National Guard soldier returns from a 10-month deployment in Kosovo to Fort Bliss, Texas, Dec. 18, 2020.
Dec. 21, 2020
On Dec. 20, 2020, the Department of Defense (DOD), in coordination with the Department of Health and Human Services (HHS), awarded an Indefinite Delivery/Indefinite Quantity contract to Anatrace Products, LLC. to support increased testing demands for COVID-19. COVID-19 diagnostics requires the key reagents Polyadenylic Acid (Poly A), Guanidinium Thiocyanate (GTC), and Proteinase K (Pro K) to process samples. Supply chain analysis has identified the severe impact of the limited availability of these reagents on laboratories preparing samples for SARS-CoV-2 testing.
This industrial base expansion effort, with a not-to-exceed value of $4.8 million, will allow Anatrace to increase production capacity for the three key extraction reagents (Poly A, GTC and Pro K) at their facility in Holland, Ohio. This expansion initiative will increase their current production 10-fold, with production activities beginning January 2021. Anatrace anticipates full production increases for Poly A (increase to at least 1,600 grams) and Pro K (increase to at least 100 grams) by July 2021 and for GTC (increase to 25,000 kgs) by September 2021.
DOD’s Defense Assisted Acquisition (DA2) Cell led this effort in coordination with the Department of the Air Force’s Acquisition COVID-19 Task Force (DAF ACT). The effort was funded through the Health Care Enhancement Act (HCEA) to enable and support domestic industrial base expansion for critical medical resources.
Dec. 18, 2020
Below is a compilation of initiatives, actions and accomplishments across Operation Warp Speed (OWS)’s primary efforts in the past week. To learn more about OWS, visit the Department of Health and Human Services (HHS) website and Department of Defense (DOD) website.
VACCINE DEVELOPMENT:
The U.S. Food and Drug Administration granted Emergency Use Authorization for the Pfizer COVID-19 vaccine Dec. 11. The Vaccines and Related Biological Products Advisory Committee convened Dec. 17 to review and evaluate data concerning the safety and effectiveness and appropriate use of the Moderna vaccine candidate. The committee overwhelmingly voted to recommend Emergency Use Authorization for the vaccine. The meeting was public and related material is available for independent and public review. A recommendation from the FDA is anticipated soon.
THERAPEUTICS DEVELOPMENT:
The U.S. Department of Health and Human Services continues to publish allocations for monoclonal antibody treatments. As of this week, more than 400,000 doses of monoclonal antibodies have been allocated to the states and territories. Facilities that have utilized their allocated monoclonal antibodies can request additional patient courses through their state/territory health department. If another healthcare facility does not accept or want its allocated amount, those patient courses can be reallocated by the state to other healthcare facilities within their jurisdiction.
MANUFACTURING, DISTRIBUTION AND ADMINISTRATION:
The Advisory Committee on Immunization Practices (ACIP) issued interim considerations recommending the Pfizer vaccine for people 16 years and older. The clinical considerations are informed by FDA-submitted data, best practice guidelines and expert opinion.
Pfizer vaccine distribution began within 24 hours of the FDA granting Emergency Use Authorization. More than 1,500 individual shipments were delivered in the first week. Pfizer will continue to ship its product weekly, fulfilling orders among 64 jurisdictions and five federal entities. The Operation Warp Speed feature page includes updated photos.
KEY ENGAGEMENTS/OUTREACH:
HHS Secretary Azar joined the National Ceremonial COVID-19 Vaccination Kick Off Event with Surgeon General Jerome Adams on Monday, December 14, and visited another hospital to see more frontline healthcare workers receive vaccinations on Wednesday, December 16.
Operation Warp Speed Deputy Director of Supply, Production and Distribution Maj. Gen. Chris Sharpsten and Deputy Secretary of the Department of Health and Human Services Eric Hargan visited the Washington, D.C. Veterans Affairs Medical Center as the first doses of the Pfizer COVID-19 vaccine were administered to healthcare workers.
Operation Warp Speed’s Supply, Production and Distribution Deputy Chief Marion Whicker and Manufacturing lead Col. Mike Post conducted
quality checks at Pfizer’s plant in Kalamazoo, Michigan, observing the
pick-and-pack process, and following a vaccine shipment from the plant
to an administration site.
Operation Warp Speed will hold a press conference following any
announcements granting EUA for the Moderna vaccine. Sign up for email updates.
SENIOR LEADER QUOTES:
“It is nothing short of a medical miracle to have FDA authorization of a vaccine for COVID-19 just over 11 months since the virus was made known to the world. This vaccine, like any vaccine FDA potentially authorizes, has been through multiple stages of safety review, and it has shown extraordinary effectiveness in protecting people from the virus. Vaccines will help bring this pandemic to an end, which is all the more reason to double down on the public health measures we need to stay safe in the coming months.” ~ U.S. Secretary of Health and Human Services Alex Azar
“Fortunately for the nation, some of the greatest logistical minds in the country are working daily at Operation Warp Speed with one goal – delivering safe and effective vaccines to the American people,” ~ Operation Warp Speed Deputy Chief Supply, Production and Distribution Marion Whicker.
“This is a monumental week for us all as we distribute the first millions of doses of vaccines to the American people. But each week that follows, we will have more doses ready for allocation and distribution. We are also posturing to phase in the Moderna vaccine, if they receive an EUA. This is about a steady cadence of delivery to bring the American people to a place of confidence that vaccine is coming. We want to ensure the vaccine arrives safely and that it can be effectively administered once arrival occurs.” ~Operation Warp Speed Chief Operating Officer GEN Gus PernaDec. 18, 2020
Today, the Department of Defense announced that
Acting Secretary Chris Miller intends to appoint former Assistant
Secretary of the Air Force (Manpower & Reserve Affairs) Tidal McCoy
and former NASA CFO Jeff DeWit to the Defense Science Board (DSB).
“The Defense Science Board has a long and storied history of providing
senior leaders advice on some of the most complex tech issues facing our
nation and we’re proud to have Mr. McCoy and Mr. DeWit join the board,”
said Dave Vasquez, a Department of Defense Spokesman. “Both of these
patriotic Americans have a distinguished record of public service at
senior levels of the Department of Defense and NASA respectively.”
About the Defense Science Board
The Defense Science Board provides independent advice and recommendations on matters concerning science, technology, manufacturing and acquisition processes which support the Department of Defense’s (DoD) scientific and technical enterprise.
|
NIJ announced almost $17 million in funding to support 36 forensic science research and development projects in fiscal year 2020 under its Research and Development in Forensic Science for Criminal Justice Purposes (Forensic Science R&D) program. Through its R&D grant funding, NIJ continues to advance the speed, accuracy, and reliability of forensic analysis, which ultimately bolsters the administration of justice. REVIEW AWARDS |